- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
9 月 . 17, 2024 08:01 Back to list
Best Antibiotic for Lung Infection - Comprehensive Guide
What is the Best Antibiotic for a Lung Infection?
Lung infections, commonly known as pneumonia, can have various causes, including bacterial, viral, and fungal pathogens. Bacterial pneumonia is often treated with antibiotics. However, choosing the best antibiotic depends on several factors, including the type of bacteria causing the infection, the patient’s medical history, and local antibiotic resistance patterns.
Understanding Lung Infections
Pneumonia primarily occurs when bacteria, viruses, or fungi invade lung tissues, leading to inflammation and filling of the air sacs with fluid or pus. The most common bacterial causes include Streptococcus pneumoniae and Haemophilus influenzae. Less frequently, other bacteria such as Legionella pneumophila and Staphylococcus aureus can cause pneumonia, particularly in people with weakened immune systems.
Diagnosis
Diagnosing a lung infection involves a thorough medical history, physical examination, and diagnostic tests such as chest X-rays and sputum cultures. The results determine the causative organism and help guide appropriate antibiotic therapy. It is crucial to collect these samples before initiating antibiotic treatment to identify the specific pathogen effectively.
Common Antibiotics
The first-line antibiotics for community-acquired pneumonia typically include macrolides (such as azithromycin) and beta-lactams (such as amoxicillin) for healthy adults
. In cases of more severe pneumonia or in patients with coexisting conditions, respiratory fluoroquinolones (like levofloxacin) or high-dose beta-lactam regimens may be recommended.what is the best antibiotic for a lung infection

For hospital-acquired pneumonia, the choice of antibiotic is more complex due to the higher likelihood of multi-drug resistant organisms. In such instances, a combination of antibiotics may be required to cover a broader range of potential pathogens. Options may include piperacillin-tazobactam, cefepime, or meropenem, depending on the specific bacteria suspected.
Factors Influencing Antibiotic Choice
1. Type of Infection The specific bacteria involved dictate the choice of antibiotic. Culture results can provide targeted therapy but may take time. 2. Patient Health Young, healthy individuals may respond well to standard treatments, while older adults or those with chronic diseases may require more aggressive therapy and broader coverage.
3. Local Resistance Patterns Antibiotic resistance is a growing concern, and local healthcare providers typically have access to resistance data, allowing them to make informed decisions.
4. Allergies and Side Effects Patients with known allergies to antibiotics must be managed cautiously, ensuring that alternative medications are both effective and safe.
Conclusion
There is no single “best” antibiotic for all lung infections; the most effective treatment depends on the nature of the infection, patient factors, and local resistance patterns. It's crucial for healthcare providers to evaluate each case individually and modify treatment based on clinical response and laboratory results. Patients should also be aware of the importance of completing their antibiotic course to ensure full recovery and mitigate the risks of developing antibiotic resistance. If symptoms of pneumonia arise, such as cough, fever, and difficulty breathing, seeking medical attention promptly can lead to better outcomes and recovery. Always consult a healthcare professional before starting any medication.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
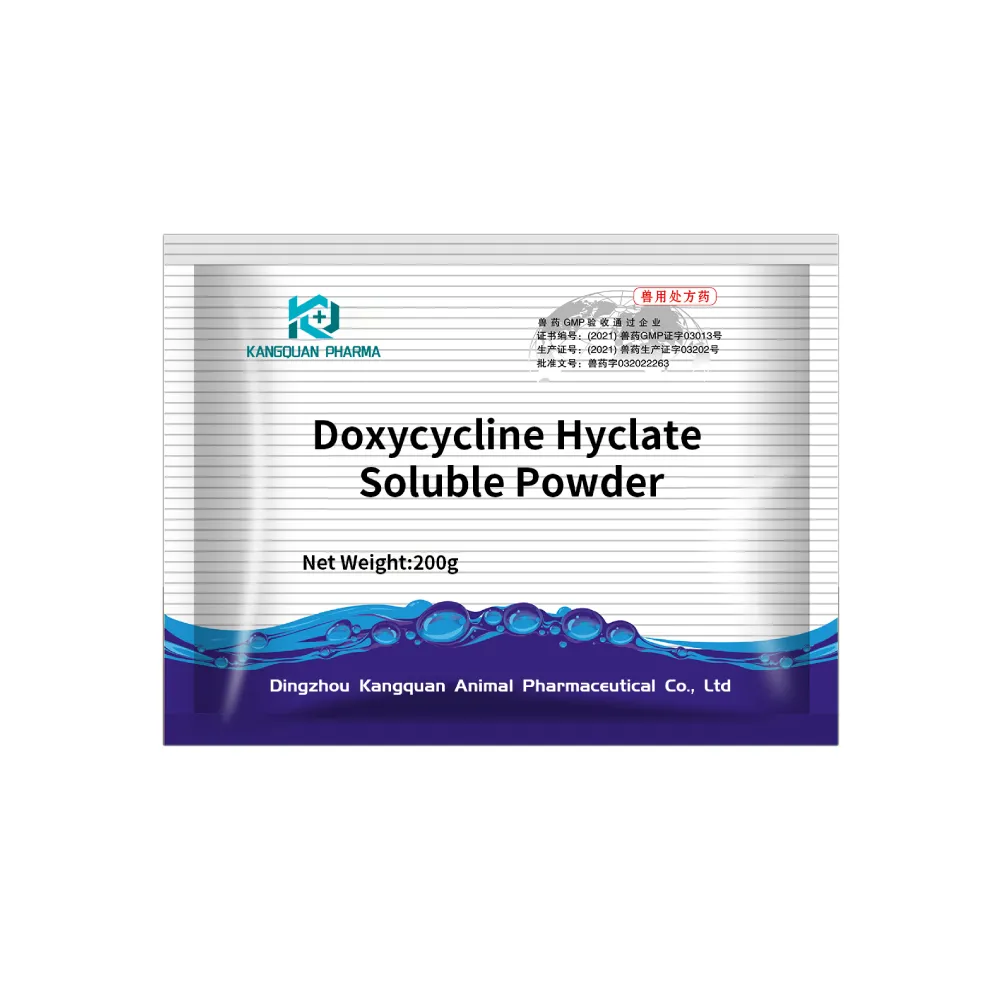
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024