- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
7 月 . 25, 2024 11:26 Back to list
Understanding the Various Mechanisms Behind Antibiotic Resistance in Bacteria and Their Implications
Mechanisms of Antibiotic Resistance An Overview
Antibiotic resistance is a pressing global health concern that poses significant challenges to the treatment of infectious diseases. The emergence of resistant strains of bacteria limits the effectiveness of antibiotics, resulting in prolonged illness, increased medical costs, and a higher mortality rate. Understanding the mechanisms of antibiotic resistance is crucial for developing strategies to combat these resistant pathogens.
Mechanisms of Antibiotic Resistance An Overview
Another significant mechanism is the acquisition of resistance genes via horizontal gene transfer (HGT). This process allows bacteria to gain resistance traits from other bacteria, even across different species. There are three main methods of HGT transformation, transduction, and conjugation. Transformation involves the uptake of naked DNA from the environment, while transduction requires bacteriophages to transfer genetic material between bacteria. Conjugation, the most common method, involves plasmids—circular DNA molecules that can replicate independently—being directly transferred from one bacterium to another through physical contact. This exchange allows for the rapid spread of resistance traits within bacterial populations, making it a formidable challenge in controlling infections.
mechanisms of antibiotic resistance pdf

Furthermore, bacteria can actively expel antibiotics from their cells through efflux pumps. These specialized protein complexes can recognize and transport a wide range of antimicrobial agents out of the cell, decreasing the intracellular concentration of the drug and diminishing its effectiveness. Efflux pumps can be specific to certain classes of antibiotics or can have broad-spectrum activity, further complicating treatment options.
Additionally, some bacteria possess enzymes that can inactivate antibiotics before they can exert their effects. For example, beta-lactamases are enzymes produced by certain bacteria that can break down the beta-lactam ring structure of penicillin and its derivatives. This enzymatic breakdown renders the antibiotic ineffective and allows the bacteria to survive and reproduce in its presence. The production of such enzymes is often encoded by plasmids, enhancing the potential for rapid spread among bacterial populations.
Biofilm formation is another critical factor contributing to antibiotic resistance. Many bacteria can adhere to surfaces and form biofilms, organized communities encased in a protective extracellular matrix. This biofilm environment can significantly limit the penetration of antibiotics, making it challenging to eradicate the bacteria. Moreover, the slow-growing cells within biofilms may be less susceptible to antibiotics that target rapidly dividing bacteria.
In conclusion, the mechanisms of antibiotic resistance are multifaceted, involving genetic mutations, horizontal gene transfer, efflux pumps, enzymatic inactivation, and biofilm formation. The combination of these factors contributes to the survival and persistence of resistant strains in clinical settings. Addressing antibiotic resistance requires a multifaceted approach, including the development of new antibiotics, combination therapies, and robust infection control measures. Promoting responsible antibiotic use and investing in research to understand and combat resistance mechanisms are essential steps toward safeguarding global health and ensuring the efficacy of antibiotics for future generations.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
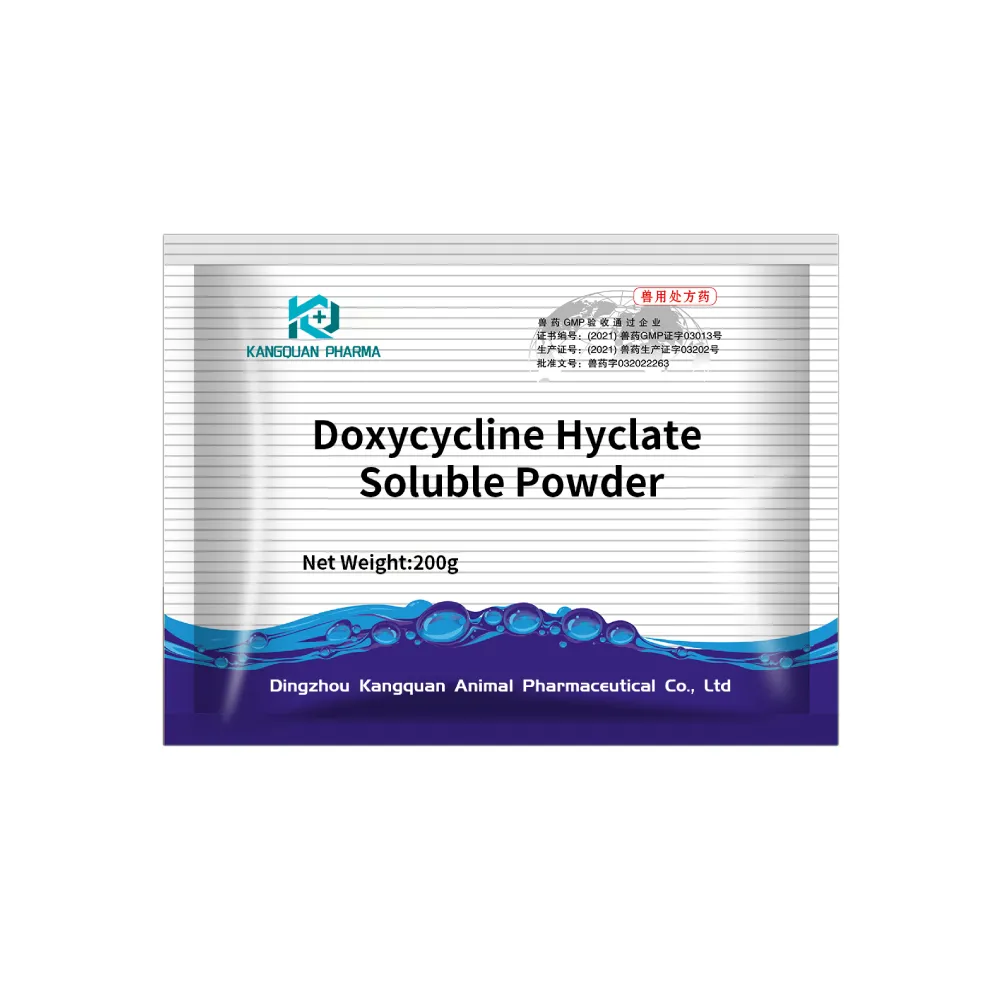
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024