- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
9 月 . 30, 2024 09:05 Back to list
Essential Guide to Antibiotic Pharmacotherapy for Effective Treatment Strategies
A Pocket Guide to Antibiotic Pharmacotherapy
Antibiotic pharmacotherapy is a crucial component of modern medicine, playing a vital role in the treatment of bacterial infections. The development and appropriate use of antibiotics have transformed infectious disease management, dramatically reducing morbidity and mortality rates associated with once-deadly diseases. This article outlines key principles, common classes of antibiotics, mechanisms of action, resistance issues, and guidelines for effective antibiotic use.
Principles of Antibiotic Use
The primary objective of antibiotic therapy is to eradicate the infection while minimizing potential side effects and resistance development. Before initiating therapy, it is essential to consider several factors
1. Microbial Identification Whenever possible, specimens should be obtained for microbiological culture prior to starting antibiotics. This aids in identifying the pathogen and determining its susceptibility.
2. Empirical vs. Targeted Therapy In many cases, empirical therapy—administering broad-spectrum antibiotics based on clinical guidelines—is necessary, especially in severe cases. Once culture results are available, antibiotics should be narrowed to targeted therapy to reduce side effects and resistance.
3. Pharmacokinetics and Pharmacodynamics Understanding how antibiotics work in the body helps in selecting the appropriate drug and dosage. Key concepts include
- Absorption The route of administration can affect the efficacy of the drug. - Distribution Antibiotics must reach adequate concentrations at the site of infection. - Metabolism and Excretion These factors dictate the dosing schedule and duration of therapy.
Common Classes of Antibiotics
Antibiotics are classified into different groups based on their chemical structure and mode of action. Some of the most commonly used classes include
- Beta-Lactams This group includes penicillins, cephalosporins, and carbapenems. They inhibit cell wall synthesis, making them highly effective against many Gram-positive and some Gram-negative bacteria.
- Macrolides Drugs like azithromycin and clarithromycin that inhibit bacterial protein synthesis and are effective against a variety of organisms, including atypical pathogens.
- Fluoroquinolones Such as ciprofloxacin and levofloxacin, these drugs inhibit DNA gyrase and topoisomerase IV, making them useful for a wide range of infections, although resistance is emerging.
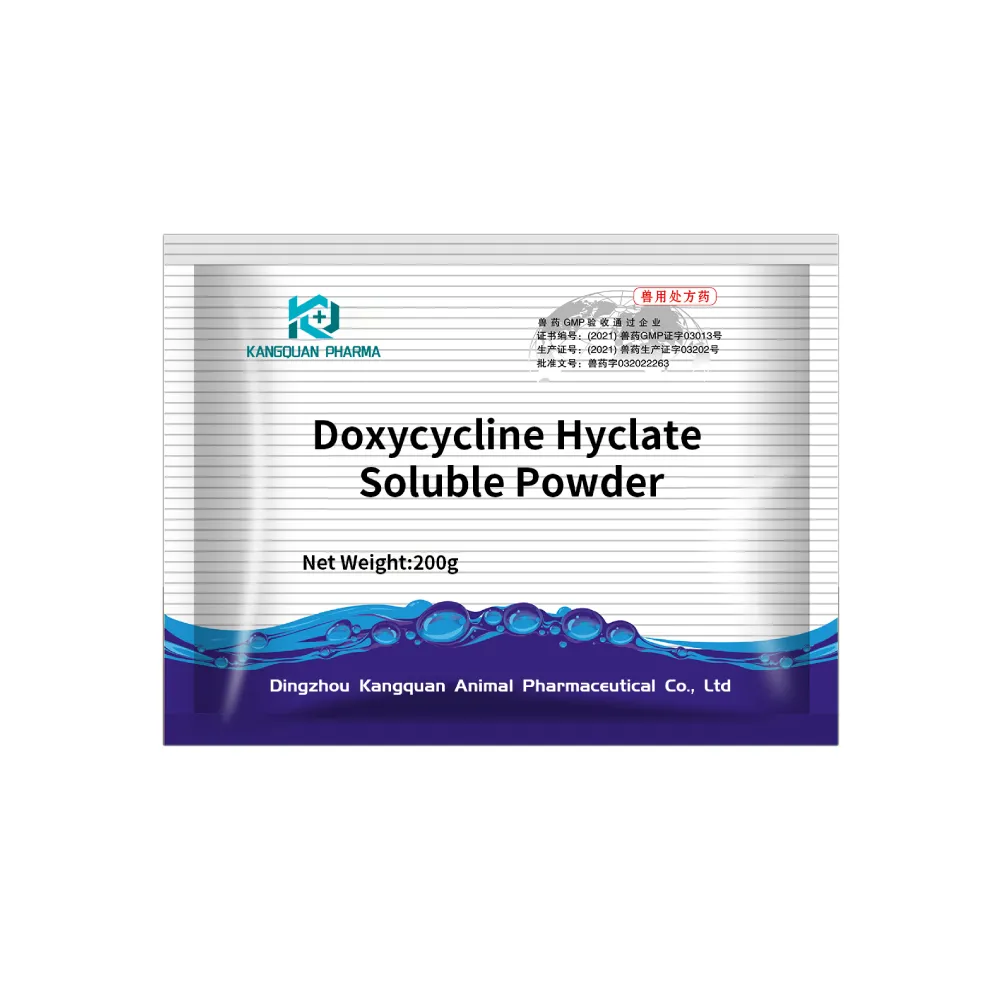
- Tetracyclines These antibiotics, including doxycycline, are effective against both Gram-positive and Gram-negative bacteria, as well as certain atypical pathogens.
pocket guide for antibiotic pharmacotherapy

- Glycopeptides Vancomycin is a primary example, used to treat serious infections caused by Gram-positive bacteria, especially methicillin-resistant Staphylococcus aureus (MRSA)
.Antibiotic Resistance
Antibiotic resistance is a significant public health concern, exacerbated by the overuse and misuse of antibiotics. Mechanisms of resistance can include
1. Enzymatic Degradation Some bacteria produce enzymes that inactivate antibiotics.
2. Altered Target Sites Mutations in bacteria can change the target sites of antibiotics, rendering them ineffective.
3. Efflux Pumps Many bacteria can pump out antibiotics before they can exert their effects.
Preventing antibiotic resistance involves careful prescribing practices, patient education, and adherence to infection control practices.
Guidelines for Effective Antibiotic Therapy
To optimize antibiotic use, healthcare providers should adhere to several guidelines
- Utilize Evidence-Based Guidelines Follow local and national guidelines for empirical therapy based on site of infection and local resistance patterns.
- Limit Duration of Therapy Shorter courses of antibiotics are often as effective as longer ones for many infections, reducing the risk of resistance.
- Monitor Patient Response Regularly assess the patient's clinical response to antibiotics and modify therapy as necessary.
- Educate Patients Empower patients with knowledge about their treatment, the importance of adherence to prescribed regimens, and the risks of misuse.
In conclusion, the principles of antibiotic pharmacotherapy hinge on accurate diagnosis, empirical and targeted therapy, and an understanding of pharmacokinetics, all underpinned by a commitment to combating resistance. By adopting best practices and guidelines, healthcare providers can help ensure effective treatment of bacterial infections while safeguarding the efficacy of antibiotics for future generations.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024