- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
9 月 . 16, 2024 09:27 Back to list
pocket guide for antibiotic pharmacotherapy
Understanding Antibiotic Pharmacotherapy A Pocket Guide
Antibiotic pharmacotherapy is a critical component of modern medicine, instrumental in treating bacterial infections and improving patient outcomes. As resistance to antibiotics grows, the need for effective strategies in antibiotic use becomes paramount. This article provides an overview of essential principles and practices in antibiotic pharmacotherapy, drawing insights from the Pocket Guide for Antibiotic Pharmacotherapy.
Key Principles of Antibiotic Use
When prescribing antibiotics, it's vital to choose the right agent for the specific infection while considering the patient's individual circumstances. The selection process begins with understanding the type of bacteria responsible for the infection. Proper microbiological testing, including culture and susceptibility testing, allows clinicians to identify the causative pathogens and select the most effective antibiotic.
Broad-Spectrum vs
. Narrow-Spectrum AntibioticsOne of the cornerstone concepts in antibiotic therapy is the distinction between broad-spectrum and narrow-spectrum antibiotics. Broad-spectrum antibiotics are effective against a wide variety of bacteria and are often used when the pathogen is unknown. However, their indiscriminate use can lead to collateral damage, affecting the body’s normal flora and potentially leading to antibiotic resistance. Conversely, narrow-spectrum antibiotics target specific types of bacteria and should be favored when the responsible organism is known, minimizing the risk of resistance.
pocket guide for antibiotic pharmacotherapy

Dosing Strategies and Pharmacokinetics
Understanding pharmacokinetics—the study of how drugs are absorbed, distributed, metabolized, and excreted—is crucial for effective antibiotic therapy. Factors such as age, kidney function, and weight can impact drug levels in the body. Therefore, dosage adjustments may be necessary to ensure efficacy while minimizing toxicity. The guide emphasizes that clinicians must consider the pharmacodynamics as well, which examines how antibiotics affect bacteria over time.
Monitoring and Side Effects
Regular monitoring of the patient’s response to therapy is essential. Signs of treatment failure or adverse effects can indicate the need for changes in therapy. Common side effects of antibiotics include gastrointestinal disturbances and allergic reactions, and the increasing incidence of Clostridioides difficile infections is a significant concern linked to antibiotic use. Therefore, practitioners must educate patients on potential side effects and symptoms that warrant immediate medical attention.
Conclusion
Antibiotic pharmacotherapy is an evolving field, and healthcare professionals must stay informed of current guidelines and resistance patterns. The Pocket Guide for Antibiotic Pharmacotherapy serves as a valuable resource, aiding practitioners in optimizing antibiotic use while combating the growing threat of resistance. By adhering to evidence-based practices, clinicians can improve treatment outcomes and promote responsible antibiotic stewardship, ultimately preserving the efficacy of these vital medications for future generations.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
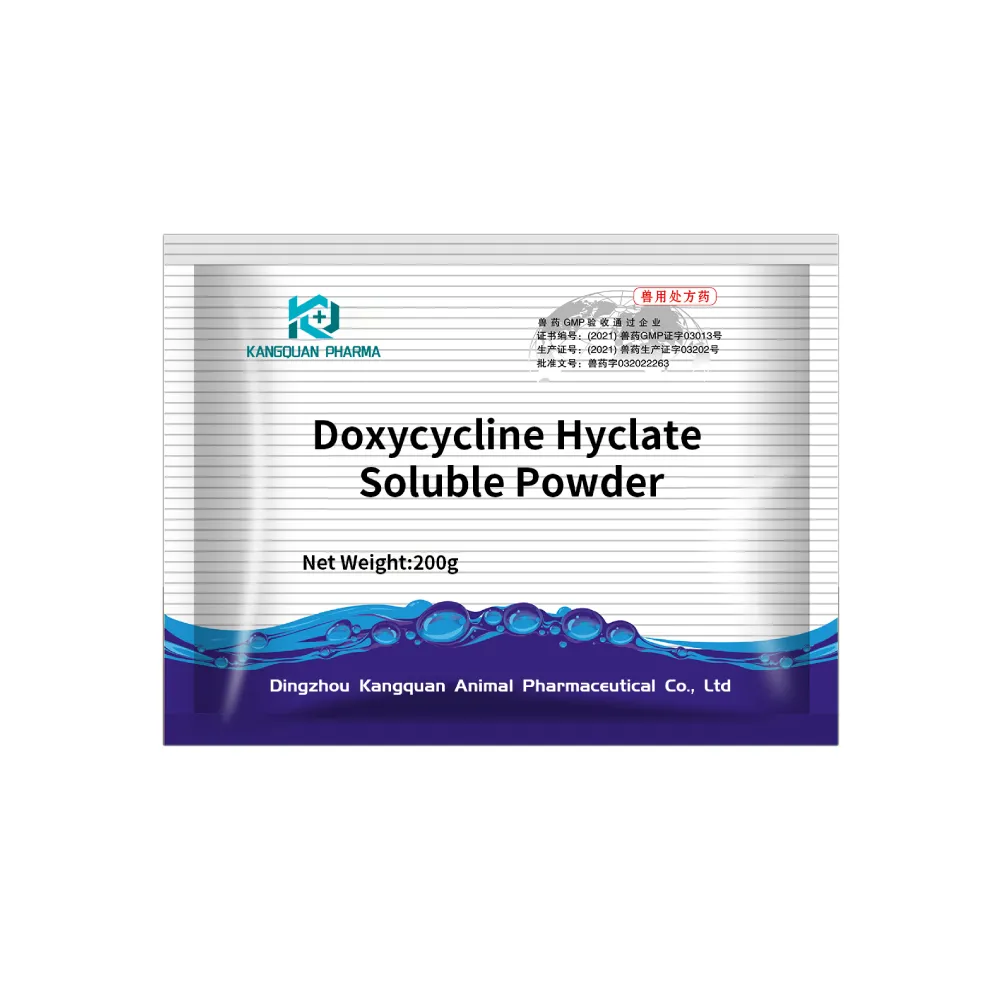
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024