- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
2 月 . 18, 2025 04:29 Back to list
can you inject ivermectin


When approached about the potential of ivermectin injections, it is vital to rely on expert discussions and peer-reviewed scientific literature for guidance. Health professionals unanimously discourage off-label therapies that include injecting ivermectin without established efficacy and safety profiles. Misuse can lead to severe health complications, enforcing the narrative that unauthorized medical practices can be perilous. From an experiential viewpoint, anecdotal instances around the unauthorized use of ivermectin injectables, often magnified by misinformation, highlight critical public health challenges. Unsubstantiated claims have led some individuals to pursue unverified treatment plans, ultimately undermining their health and drawing concerns from the medical community. These stories serve as a precautionary tale, demonstrating the substantial differences between anecdote and evidence. Expert voices in pharmacology and infectious diseases underscore that treatments must adhere to evidence-based practices to establish confidence. The medical consensus maintains that ivermectin’s benefits are formulation-specific and context-dependent. Thus, its performance in an injectable form remains uncharted and unauthorized, making it an unreliable choice not aligned with professional health guidelines. Trust, a vital cornerstone in medical guidance, hinges on robust communication channels between patients and licensed health professionals. Patients are advised to seek advice directly from healthcare providers and inquire about FDA-recognized therapeutic options tailored to their health needs, to avoid the pitfalls of unsanctioned medical use. In conclusion, can ivermectin be injected? While theoretically plausible, its injection into humans remains outside validated medical practices and lacks endorsement from health authorities. Sound health decisions are rooted in expert consultations, peer-reviewed research, and regulatory adherence. The case of ivermectin injections underlines a broader narrative on the importance of basing health-related choices on credibility and scientific evidence.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
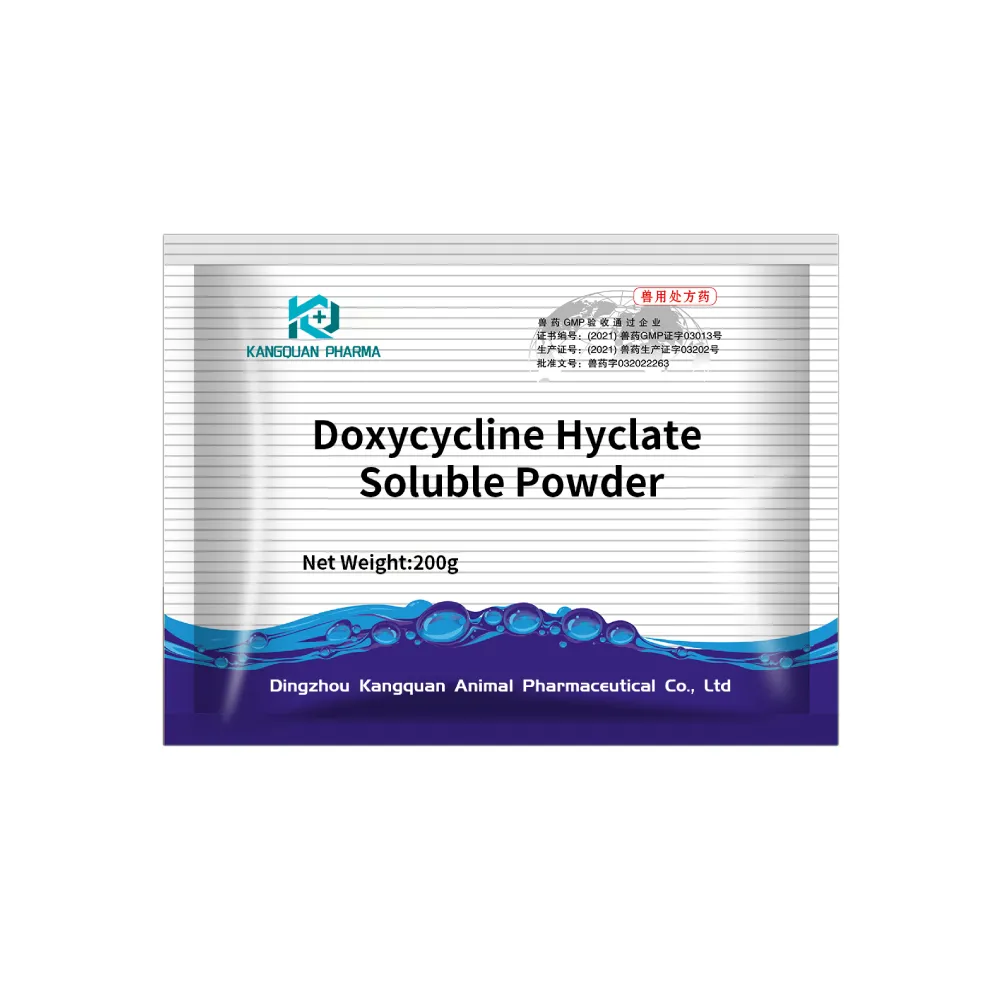
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024