- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
10 月 . 30, 2024 17:11 Back to list
antimicrobial resistance mechanisms pdf
Understanding Antimicrobial Resistance Mechanisms
Antimicrobial resistance (AMR) has emerged as a global public health crisis, threatening the effectiveness of treatments for bacterial infections, fungal diseases, and even viral infections. AMR occurs when microorganisms evolve to resist the effects of medications that once successfully treated them. Understanding the mechanisms behind AMR is crucial for developing strategies to combat this growing threat.
One primary mechanism of AMR is genetic mutation. Microbes can undergo spontaneous mutations in their DNA during replication. These mutations may confer resistance to specific antibiotics. For instance, mutations in the genes coding for bacterial ribosomes can prevent antibiotics like tetracycline from binding effectively, rendering the drug ineffective.
Another significant mechanism is the acquisition of resistance genes through horizontal gene transfer. Bacteria can exchange genetic material through processes such as conjugation, transformation, and transduction. This horizontal gene transfer allows resistant genes to spread rapidly among bacterial populations, even across different species. Plasmids, small DNA molecules that can replicate independently, often carry these resistance genes and can be easily transferred between bacteria.
Efflux pumps also play a crucial role in antimicrobial resistance. These are proteins that actively pump out antibiotics from bacterial cells, reducing the concentration of the drug to sub-lethal levels. This mechanism is particularly common in Gram-negative bacteria, which employ efflux systems to expel multiple classes of antibiotics, thereby acquiring multidrug resistance.
antimicrobial resistance mechanisms pdf

Biofilm formation is another strategy employed by bacteria to resist antimicrobial action. Bacterial biofilms are complex communities of microorganisms encased in a protective extracellular matrix. This matrix acts as a barrier that limits the penetration of antibiotics, allowing bacteria to survive in environments where the drugs would otherwise be effective. Biofilms can form on various surfaces, including medical devices and human tissues, complicating treatment efforts.
The production of enzymes that inactivate antibiotics constitutes yet another mechanism of AMR. Bacteria like Staphylococcus aureus produce beta-lactamases, enzymes that break down penicillin and cephalosporins, rendering these antibiotics ineffective. The prevalence of such enzymes is a growing concern in both healthcare and community settings, as they can arise from previously susceptible strains of bacteria.
In addition to these biological mechanisms, the overuse and misuse of antibiotics in healthcare and agriculture significantly contribute to the acceleration of AMR. In many cases, antibiotics are prescribed unnecessarily or not taken as directed, allowing bacteria to adapt and develop resistance.
Combating antimicrobial resistance requires a multifaceted approach, including the responsible use of antibiotics, increased surveillance of resistance patterns, and the development of novel therapeutic strategies. By understanding the underlying mechanisms of AMR, researchers and healthcare providers can better address this complex challenge, ensuring effective treatments remain available for future generations. Awareness and education on the importance of antibiotic stewardship are equally crucial in mitigating the impact of AMR on global health.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
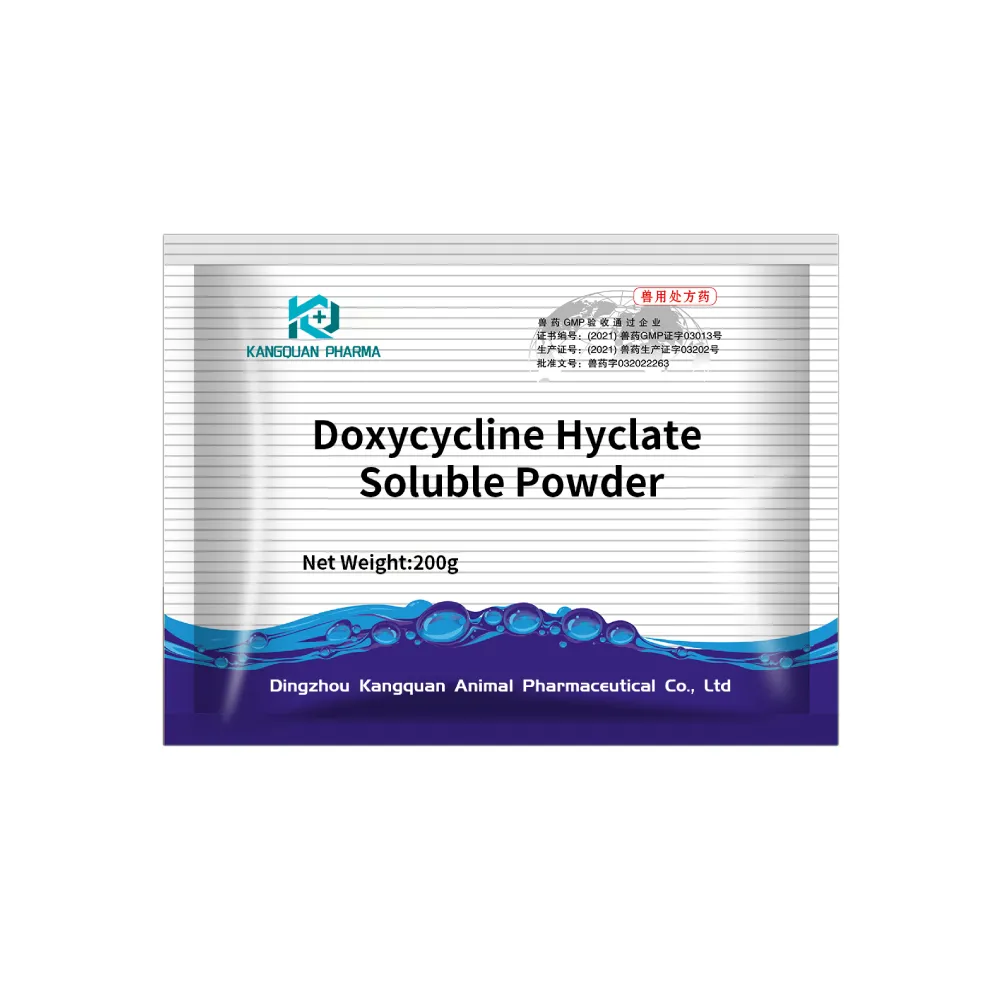
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024