- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
10 月 . 20, 2024 19:18 Back to list
antimicrobial resistance mechanisms pdf
Understanding Antimicrobial Resistance Mechanisms
Antimicrobial resistance (AMR) is a significant global health threat that arises when microorganisms—such as bacteria, viruses, fungi, and parasites—develop resistance to antimicrobial agents that were once effective in treating them. This phenomenon poses challenges not only to effective disease management but also to public health at large. Understanding the mechanisms of antimicrobial resistance is crucial for developing strategies to combat this escalating problem.
One of the primary ways microorganisms develop resistance is through genetic mutations. Spontaneous mutations can occur in bacterial DNA when they replicate, leading to altered cellular functions. For example, a mutation might prevent an antibiotic from entering the bacterial cell or alter the structure of the target enzyme that an antibiotic typically inhibits. This kind of resistance mechanism can be particularly concerning in bacteria such as *Mycobacterium tuberculosis*, the causative agent of tuberculosis, which has shown increasing rates of drug resistance due to genetic changes.
Understanding Antimicrobial Resistance Mechanisms
In addition to genetic changes, bacteria can also develop resistance through physiological alterations. For example, biofilm formation is a common strategy employed by bacteria to evade the effects of antimicrobial agents. Biofilms are clusters of bacteria embedded in a self-produced matrix that adheres to surfaces. This matrix acts as a protective shield against antibiotics, making it considerably more challenging for drugs to penetrate and effectively kill the bacteria within the biofilm. Infections associated with biofilms are particularly problematic in medical implants and chronic wounds.
antimicrobial resistance mechanisms pdf

Another significant mechanism of resistance is the production of enzymes that degrade or modify antimicrobial agents. For instance, many bacteria produce beta-lactamases, enzymes that break down beta-lactam antibiotics, including penicillin and cephalosporins. The emergence of bacteria that produce extended-spectrum beta-lactamases (ESBLs) or carbapenemases has led to severe treatment failures, as these enzymes can inactivate a broad range of antibiotics. Research has shown that the overuse and misuse of antibiotics in both human medicine and agriculture have accelerated the development and spread of these enzyme-producing bacteria.
Efflux pumps are also critical players in antimicrobial resistance. These membrane-based protein structures actively expel antibiotics and other toxic substances from inside the bacterial cell, thereby reducing drug concentration to ineffective levels. Some bacteria possess multi-drug efflux pumps that can remove a variety of antibiotics simultaneously, contributing to a resistant phenotype. This mechanism is particularly prevalent in Gram-negative bacteria, where the outer membrane acts as a barrier, making it essential for the efflux pumps to function effectively to resist ongoing treatment efforts.
Lastly, target modification is a sophisticated resistance strategy wherein bacteria change the target sites of antibiotics. By altering the structure of ribosomes or penicillin-binding proteins, bacteria can effectively nullify the action of the antibiotics designed to inhibit them. This mechanism is observed in various pathogens, including *Staphylococcus aureus*, which has developed strains resistant to methicillin (MRSA) through such modifications.
In conclusion, antimicrobial resistance is a multi-faceted issue involving various mechanisms that allow pathogens to survive the effects of antimicrobial agents. Understanding these mechanisms is vital for informing treatment protocols, developing new antibiotics, and implementing effective public health strategies to combat AMR. Awareness and responsible use of existing antibiotics, investment in research for novel therapeutics, and preventive measures are essential in curtailing the spread of resistant infections. Addressing antimicrobial resistance requires a coordinated effort from healthcare providers, policymakers, and the general public to ensure a healthier future.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
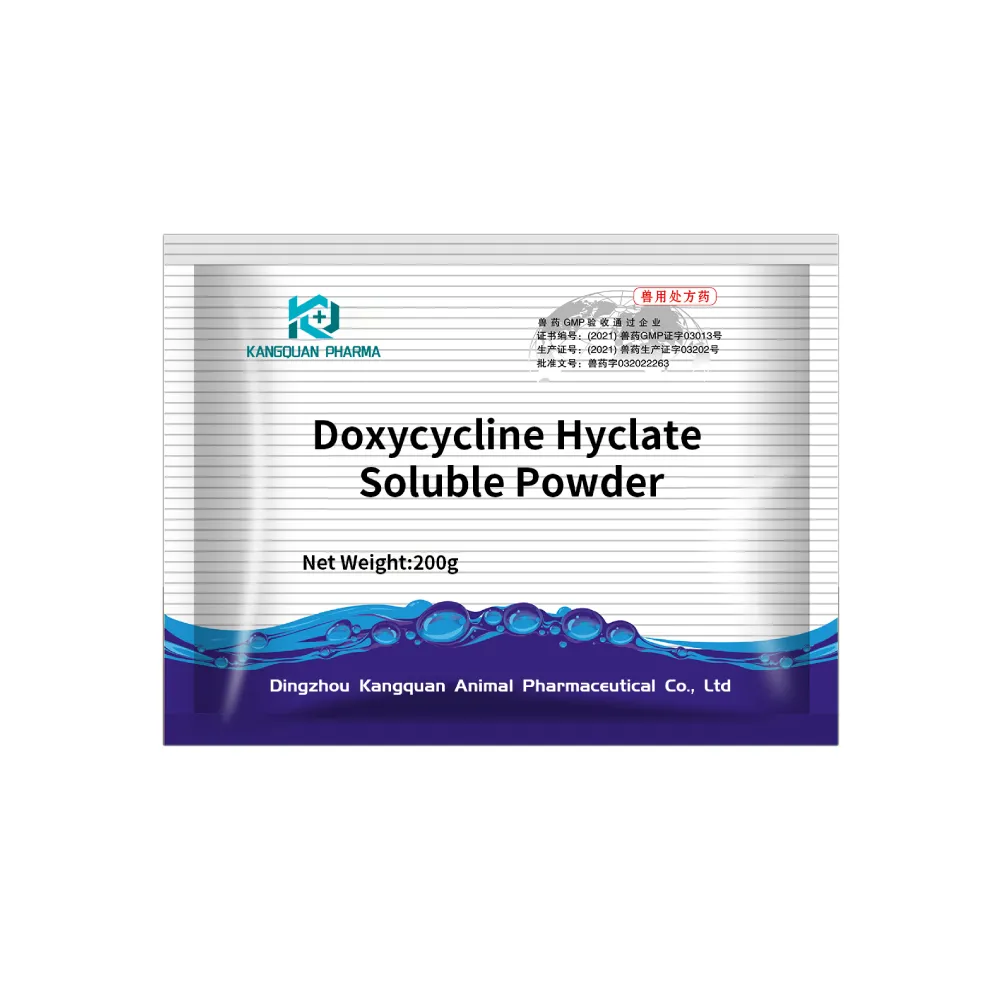
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024