- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
9 月 . 22, 2024 00:44 Back to list
antimicrobial drugs pharmacology pdf
Antimicrobial drugs play a crucial role in modern medicine by preventing and treating infections caused by various microorganisms, including bacteria, viruses, fungi, and parasites. These drugs, classified into several categories based on their spectrum of activity and mechanism of action, have revolutionized healthcare, saving countless lives since their discovery.
The pharmacology of antimicrobial drugs involves understanding their absorption, distribution, metabolism, and excretion (ADME), which influences their efficacy and safety. For instance, the bioavailability of an antimicrobial drug can significantly affect its concentration in the body. Some drugs, like penicillin, are best administered intravenously due to their poor gastrointestinal absorption, while others, such as azithromycin, can be taken orally with good bioavailability.
The mechanism of action of antimicrobial drugs varies widely. Beta-lactam antibiotics, including penicillins and cephalosporins, work by inhibiting bacterial cell wall synthesis, leading to cell lysis and death. In contrast, tetracyclines interfere with protein synthesis by binding to the bacterial ribosome, while fluoroquinolones inhibit DNA gyrase and topoisomerase, vital for bacterial DNA replication. Understanding these mechanisms is essential for predicting resistance patterns and selecting the most appropriate therapy.
The development of antimicrobial resistance (AMR) poses a significant challenge in the field of infectious diseases. Overuse and misuse of these drugs in humans and agriculture have accelerated the emergence of resistant strains. For example, Methicillin-resistant Staphylococcus aureus (MRSA) highlights the critical need for judicious use of antibiotics and the importance of surveillance programs to monitor resistance trends.
antimicrobial drugs pharmacology pdf

Combination therapy is often employed to enhance efficacy and limit resistance development. For instance, using a beta-lactam antibiotic together with an aminoglycoside can have a synergistic effect against specific infections, such as nosocomial pneumonia. Furthermore, dosing regimens and optimization strategies, including population pharmacokinetics and pharmacodynamics (PK/PD) relationships, are crucial in maximizing therapeutic outcomes while minimizing toxicity.
In the realm of pharmacology, ongoing research focuses on discovering novel antimicrobial agents, particularly those effective against multidrug-resistant organisms
. These efforts include the exploration of bacteriophage therapy, antimicrobial peptides, and agents targeting specific bacterial virulence factors.In conclusion, the pharmacology of antimicrobial drugs is a dynamic and essential aspect of medical science. As we face the growing challenge of antimicrobial resistance, the continued development, appropriate use, and innovative strategies in treating infections will be paramount to preserving the efficacy of these critical medications in healthcare. Understanding the pharmacological principles governing these agents is vital for clinicians to make informed decisions in managing infectious diseases effectively.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
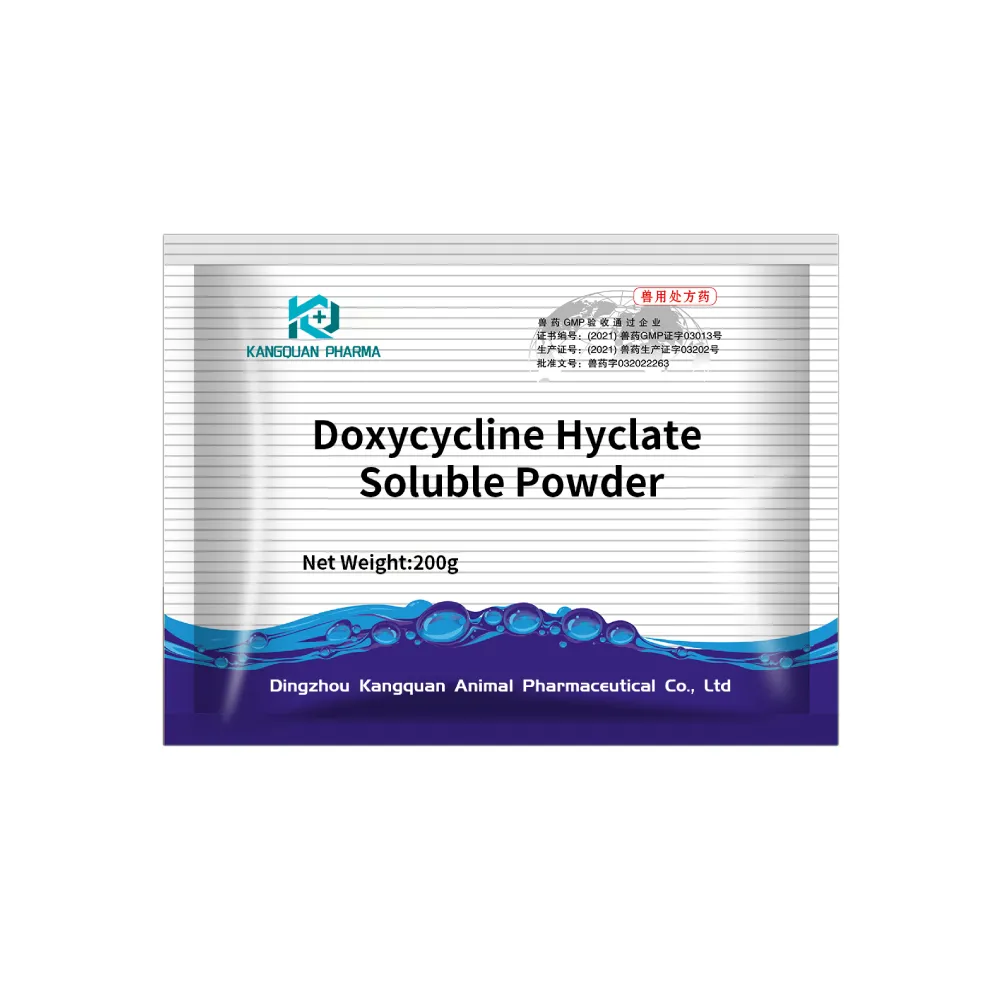
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024