- Afrikaans
- Albanian
- Amharic
- Arabic
- Armenian
- Azerbaijani
- Basque
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Catalan
- Cebuano
- Corsican
- Croatian
- Czech
- Danish
- Dutch
- English
- Esperanto
- Estonian
- Finnish
- French
- Frisian
- Galician
- Georgian
- German
- Greek
- Gujarati
- Haitian Creole
- hausa
- hawaiian
- Hebrew
- Hindi
- Miao
- Hungarian
- Icelandic
- igbo
- Indonesian
- irish
- Italian
- Japanese
- Javanese
- Kannada
- kazakh
- Khmer
- Rwandese
- Korean
- Kurdish
- Kyrgyz
- Lao
- Latin
- Latvian
- Lithuanian
- Luxembourgish
- Macedonian
- Malgashi
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Myanmar
- Nepali
- Norwegian
- Norwegian
- Occitan
- Pashto
- Persian
- Polish
- Portuguese
- Punjabi
- Romanian
- Russian
- Samoan
- Scottish Gaelic
- Serbian
- Sesotho
- Shona
- Sindhi
- Sinhala
- Slovak
- Slovenian
- Somali
- Spanish
- Sundanese
- Swahili
- Swedish
- Tagalog
- Tajik
- Tamil
- Tatar
- Telugu
- Thai
- Turkish
- Turkmen
- Ukrainian
- Urdu
- Uighur
- Uzbek
- Vietnamese
- Welsh
- Bantu
- Yiddish
- Yoruba
- Zulu
9 月 . 30, 2024 12:03 Back to list
Optimizing Antibiotic Use for Enhanced Patient Outcomes and Public Health Safety
Antibiotic Stewardship A Crucial Measure for Public Health
Antibiotic stewardship refers to a set of coordinated strategies designed to improve the use of antibiotic medications with the goal of enhancing patient outcomes, reducing microbial resistance, and decreasing the spread of infections caused by multi-drug resistant organisms. As antibiotic resistance becomes an increasingly pressing global health issue, the importance of effective antibiotic stewardship programs (ASPs) cannot be overstated.
The Growing Concern of Antibiotic Resistance
Antibiotic resistance is a natural phenomenon that occurs when bacteria evolve in response to the exposure to antibiotics. However, the misuse and overuse of these medications have accelerated this process, leading to strains of bacteria that are resistant to multiple antibiotics. According to the World Health Organization (WHO), antimicrobial resistance could lead to 10 million deaths per year by 2050 if current trends continue. Such statistics highlight the urgency of implementing robust stewardship programs within healthcare systems worldwide.
Goals and Components of Antibiotic Stewardship Programs
The primary goals of antibiotic stewardship programs are to improve patient care, ensure the efficacy of antibiotics, and minimize the negative consequences associated with their use. An effective ASP consists of several key components
1. Leadership Commitment Successful implementation of an ASP requires a commitment from leadership within healthcare institutions. This includes the allocation of resources necessary for program development and sustainability.
2. Accountability Designating a leader or a team responsible for the stewardship program helps ensure accountability for its functioning and outcomes. This team should ideally include a physician with infectious disease expertise, a pharmacist, and a data analyst.
3. Monitoring and Reporting Collecting and analyzing data related to antibiotic prescribing patterns and patient outcomes is essential. Regular reporting of this data to healthcare providers helps identify areas for improvement and track progress.
4. Education and Training Continuous education for healthcare providers about the principles of antibiotic prescribing is critical. This includes updated guidelines, the importance of diagnostic testing, and alternative treatment options.
antibiotic stewardship pdf

5. Guideline Development Developing clinical guidelines based on the latest evidence can assist healthcare providers in making informed decisions regarding antibiotic use. These guidelines should be easily accessible and integrated into electronic health records.
6. Intervention Strategies Implementing specific interventions, such as prior authorization for certain antibiotics or automatic stop orders for certain prescriptions, can help curb inappropriate use.
The Role of Healthcare Professionals
Healthcare professionals play a crucial role in the effectiveness of antibiotic stewardship programs. Physicians must critically evaluate each clinical situation to determine whether an antibiotic is necessary, and if so, which one is most appropriate. Pharmacists can aid in this process by providing insights into antibiotic pharmacology, potential adverse effects, and interactions with other medications. Additionally, all members of the healthcare team must be proactive in educating patients about the proper use of antibiotics and the risks associated with their misuse.
Patient Engagement and Public Awareness
Engaging patients in their health care is vital for the success of antibiotic stewardship efforts. Educational initiatives aimed at the general public can help raise awareness about the dangers of antibiotic misuse, such as the importance of not demanding antibiotics for viral infections like the common cold.
Public health campaigns that promote hygiene practices, vaccination, and responsible antibiotic use can further contribute to reducing the incidence of infections and the consequent need for antibiotics.
Conclusion
Antibiotic stewardship is an essential component of modern medicine that safeguards the future effectiveness of antibiotics. Through careful implementation of stewardship programs, healthcare providers can combat the growing threat of antibiotic resistance while optimizing patient care. As we face complex global health challenges, it is crucial to foster collaborative efforts among healthcare professionals, patients, and policymakers to promote responsible antibiotic use, ultimately protecting public health for generations to come.
-
The Power of Radix Isatidis Extract for Your Health and Wellness
NewsOct.29,2024
-
Neomycin Sulfate Soluble Powder: A Versatile Solution for Pet Health
NewsOct.29,2024
-
Lincomycin Hydrochloride Soluble Powder – The Essential Solution
NewsOct.29,2024
-
Garamycin Gentamicin Sulfate for Effective Infection Control
NewsOct.29,2024
-
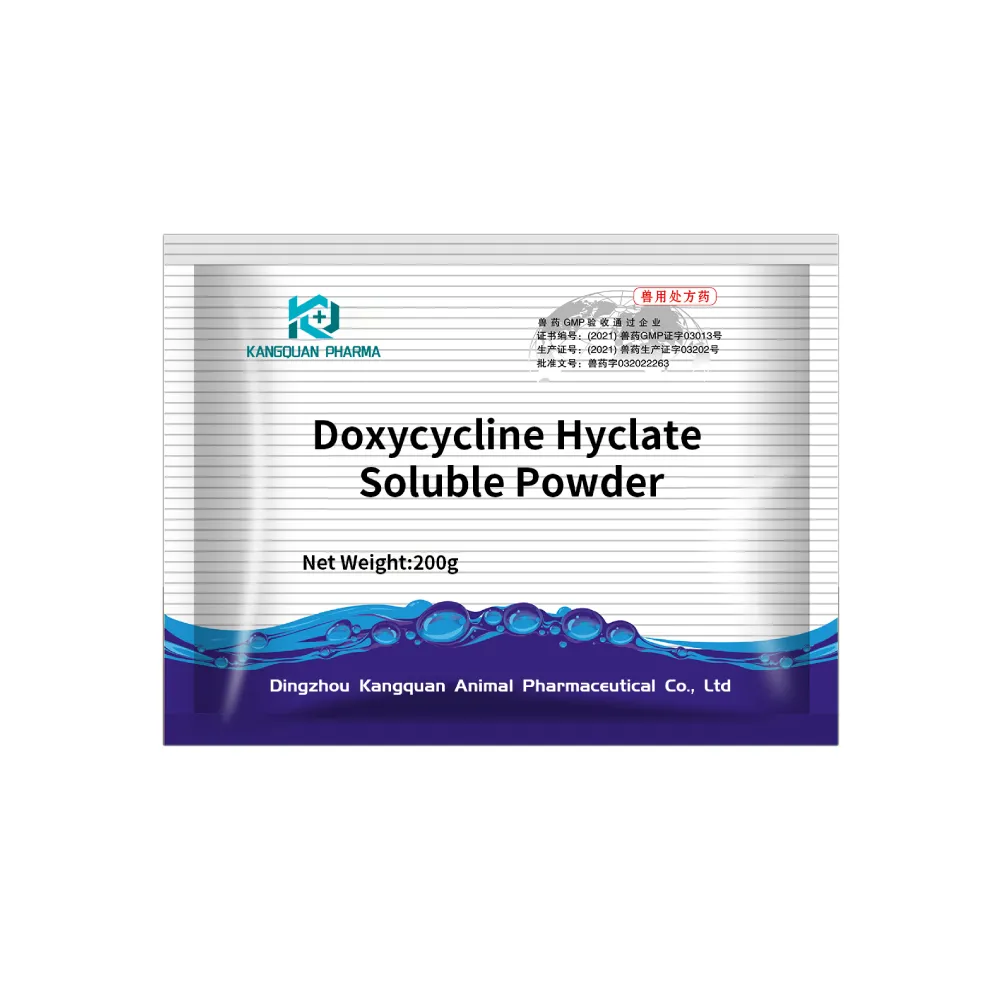
Doxycycline Hyclate Soluble Powder: Your Antibiotic Needs
NewsOct.29,2024
-
Tilmicosin Premix: The Ultimate Solution for Poultry Health
NewsOct.29,2024